Definition Rationale And Scope
Venous leg ulcers are defined as open lesions between the knee and ankle joint that occur in the presence of venous disease. They are the most common cause of leg ulcers, accounting for 60-80% of them. The prevalence of VLUs is between 0.18% and 1%. Over the age of 65, the prevalence increases to 4%. On an average 33-60% of these ulcers persist for more than 6 weeks and are therefore referred to as chronic VLUs. These ulcers represent the most advanced form of chronic venous disorders like varicose veins and lipodermatosclerosis.
Risk factors for development of VLUs include older age, female sex, obesity, trauma, immobility, congenital absence of veins, deep vein thrombosis , phlebitis, and factor V Leiden mutation.
Signs And Symptoms Of Venous Disease
- C = Clinic
| Varicosis with healed ulcus cruris venosum | |
| C 6 | Varicosis with florid ulcus cruris venosum |
There are some physical skin changes which are a sign of venous disease and obtaining early treatment should reduce discomfort. This can be heavy, tired and itchy legs, and swollen, enlarged veins appearing on the legs and feet varicose veins. The venous blood is no longer being transported to the heart properly resulting in an increased pressure within the veins commonly referred to as venous hypertension. The increased volume of blood from the incompetent veins can lead to oedema, i.e. visible and palpable collections of fluid, forming in the tissue.
C: Healed Venous Ulcer
Venous ulcers are open sores that are caused by chronic disease. Often called venous ulcers or venous stasis ulcers, they are most commonly found low on the inner ankle.
In this stage of vein disease, venous congestion is so poor that blood flow is prevented from delivering nutrition and oxygen to the skin, resulting in open sores at the surface of the skin.
Venous ulcers take a considerable amount of time to heal . Once healed, there is a risk that they can return.
Also Check: Foods That Irritate Stomach Ulcers
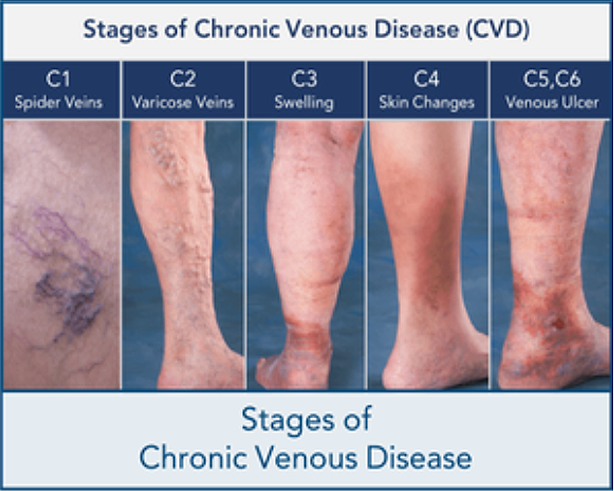
The Stages Of Chronic Venous Insufficiency
Millions of Americans suffer from vein disease, and less than 10% of people know to seek treatment.
Early stages of venous disease may not cause any noticeable symptoms. However, as the disease progresses, symptoms may become more pronounced, and even painful. In fact, without a proper diagnosis, chronic venous insufficiency may progress and lead to more long-term health problems.
The list below outlines the stages of venous insufficiency.
Important Early Warning Signs Of Venous Leg Ulcers

Leg ulcers symptoms often include a dull ache, tenderness or pain in the legs, swelling, eczema of the surrounding skin, varicose veins, and hyperpigmentation. Early signs of venous stasis ulcers include darkened or discolored skin around the ankle, or skin that feels leathery or waxy to the touch.
Many people who have untreated varicose veins wonder what causes darkening of the skin, known as hyperpigmentation. Varicose veins occur when the veins in the legs are not functioning effectively at returning blood back up to the heart. Blood begins to pool and veins swell as the pressure inside increases, often causing inflammation and redness, which can advance to brown discoloration.
This brown staining around the ankles is caused from red blood cells leaking from the veins and into the surrounding skin. The skin may become dry, itchy or leathery, and can progress into open sores or leg ulcers, creating a serious risk of bacterial infection.
Leg ulcers are often recurrent, and open ulcers can last from weeks to years with severe complications. Additionally, because they are often resistant to healing and are prone to recurrence, they can significantly increase the risks for disease or death, and also have a consequential impact on the quality of life of those who suffer from them.
Jupiter 561-625-9853 or Wellington 561-790-4550 or visit us at www.goldmanveininstitute.com.
You Might Also Enjoy…
Don’t Miss: Is Sweet Potato Good For Ulcerative Colitis
Can You Prevent Venous Insufficiency
If you have a family history of venous insufficiency, there are steps you can take to lessen your chances of developing the condition:
- Dont sit or stand in one position for long stretches of time get up and move around frequently.
- Dont smoke and if you do smoke, do everything you can to quit.
- Maintain a healthy body weight.
Take these steps to prevent the development of venous leg ulcers, especially if you are at a higher risk. Also, if an ulcer does develop, talk to your doctor right away.
About Venous Leg Ulcers
A leg ulcer is a long-lasting sore that takes more than 4 to 6 weeks to heal. They usually develop on the inside of the leg, just above the ankle.
The symptoms of a venous leg ulcer include pain, itching and swelling in the affected leg. There may also be discoloured or hardened skin around the ulcer, and the sore may produce a foul-smelling discharge.
See your GP if you think you have a leg ulcer, as it will need specialist treatment to help it heal.
Your GP will examine your leg and may carry out additional tests to rule out other conditions.
Read more about how a venous leg ulcer is diagnosed.
You May Like: Alternatives To Humira For Ulcerative Colitis
Venous Ulcer Causes And Risk Factors
Venous ulcers are caused by underlying vein disease, so improving your vein health can help you avoid getting them. To reduce your odds of developing vein disease, you may want to consider reducing any potential risk factors.
Here are a few common factors that could increase your chances of developing a venous leg ulcer:
- A sedentary lifestyle
- Pregnancy
- History of blood clots
Even with appropriate lifestyle modifications, you may still develop vein disease and venous ulcers. This is in part because there is a strong genetic component involved. If you have a close relative with vein disease, you are more likely to develop venous issues. In this case, you may wish to be closely monitored by a vein specialist to avoid any future complications.
Along with the potential development of venous leg ulcers, you may also be at increased risk for dangerous blood clots, so you should promptly seek treatment for your venous ulcers.
Causes Of Venous Ulcers
Venous ulcers most often form around the ankles.
Venous ulcers typically occur because of damage to the valves inside the leg veins. These valves control the blood pressure inside the veins. They allow it to drop when you walk. If the blood pressure inside your leg veins doesn’t fall as you’re walking, the condition is called sustained venous hypertension. That increase in blood pressure causes ulcers to form on your ankles.
Venous ulcers may also be caused by other problems with your leg veins. These include:
-
Varicose veins. These are large, bulging leg veins. They occur when valves in the leg veins dont work well, allowing blood to collect in the lower leg.
-
Chronic venous insufficiency. Like varicose veins, this condition occurs when your leg veins cant pump blood back up to your heart. Blood then pools in your lower legs, causing your legs to swell. Since the blood can’t flow well in your legs, the swelling may be extreme. This extreme swelling can put so much pressure on your skin that venous ulcers form.
Recommended Reading: Causes Of Ulcers In Horses
What Is Chronic Venous Insufficiency
Chronic venous insufficiency can develop when one-way valves in the veins are placed under ongoing strain and begin to malfunction. Both genetics and lifestyle are contributing factors. When vein valves are damaged, veins struggle against gravity to send blood back to the heart from your lower extremities. Instead of circulating efficiently, blood starts to flow backward or pool in the legs, ankles, and feet. Ultimately, this leads to the formation of varicose veins.
Common signs of chronic venous insufficiency include:
- Swelling in the legs and ankles
- Tired, aching legs
- Difficulty standing for long periods
- Non-healing wounds on your legs
- Restlessness felt especially at night
Along with causing these symptoms, untreated vein disease can place you at increased risk for dangerous health conditions like blood clots and venous ulcers . If you have signs of chronic venous insufficiency, we recommend contacting your doctor or a vein specialist as soon as possible.
Swelling In The Legs And Ankles
Venous leg ulcers are often accompanied by swelling of your feet and ankles , which is caused by fluid. This can be controlled by compression bandages.
Keeping your leg elevated whenever possible, ideally with your toes at the same level as your eyes, will also help ease swelling. You should put a suitcase, sofa cushion or foam wedge under the bottom of your mattress, to help keep your legs raised while you sleep.
You should also keep as active as possible and aim to continue with your normal activities. Regular exercise, such as a daily walk, will help reduce leg swelling. However, you should avoid standing or sitting still with your feet down. You should elevate your feet at least every hour.
Also Check: Does Stomach Ulcer Cause Pain
Symptoms Of Leg Ulcers
- that they are commonly found on the lower leg and ankle
- a sunken, asymmetrically shaped wound
- the edges of the ulcer are clearly defined from the surrounding skin
- the surrounding skin is intact, but inflamed
- the surrounding skin may be pigmented, hardened or calloused
- yellowish-white exudate
- varicose veins in the leg.
Diagnosis And Management Of Venous Leg Ulcers
Recommended Reading: What Are The Symptoms Of An Ulcer In Your Stomach
Reasons For Implementing Your Project
A lean audit demonstrated the leg ulcer service had a high number of referrals. The audit highlighted waiting lists for clinic appointments had grown to 48 weeks as existing patients were not always progressing or being referred in a timely manner. Best practice determines that a patient with a lower limb ulcer between the knee and the ankle in the presence of venous disease must be diagnosed and treated within two weeks. The audit findings showed there was no structured approach to managing leg ulcers, dressing regimes were ad-hoc with frequent regime changes, documentation did not always reflect the progression of the wound and some patients were kept in clinic for long periods without review of the diagnosis and escalation to other specialist services. Local hospital episode statistical data was above the national average6.
Further to this, patient care should be patient-centric with consideration to their physical and psychological wellbeing10,11. A patient focus group helped develop a greater understanding of how leg ulcers affected their quality of life and helped with the development of the pathway.
The tissue viability lead nurse and a leg ulcer clinical specialist received positive feedback by tissue viability nurses through a regional shared business unit and local podiatrists when using Urgostart dressings for diabetic foot ulcers. The local pilot and clinical research evidence both also showed positive outcomes if Urgostart was placed correctly.
What Are Venous Stasis Ulcers
Commonly located on the ankle or calf, venous stasis ulcers are painful and red in color but may be covered with a yellow, fibrous tissue and an irregular border.
Drainage and discharge are possible with venous stasis ulcers. This type of ulcer is common in patients with a history of leg swelling or varicose veins.
Also Check: What Foods Can I Eat If I Have An Ulcer
Skin Changes Of As An Early Stage Of Venous Disease
Some skin changes could be an indicator that you are suffering with venous disease. Look for skin discolouration , venous eczema , lipodermatosclerosis , and atrophie blanche . This stage can be described as pronounced vein weakness .As a result of impaired venous return, the venous blood flows back into the capillaries: The smallest blood vessels that provide the cells with oxygen and nutrients are also responsible for the return transportation of metabolic by-products. The capillaries of patients who suffer from chronic venous insufficiency need assistance to support their faulty veins.
Leg Ulcer Differential Diagnosis And Misdiagnosis
The development of leg ulcers is a clinical sign shared by many diseases. Leg ulcers usually occur in the lower leg or in the foot, with a predominance of venous ulcers located in the gaiter region, near the skin area affected by lipodermatosclerosis or white atrophy , and non-venous ulcers in the foot area.
Chronic wounds of the lower extremities could be sustained by several local and systemic causative factors, leading to a broad comparison among ulcers.
It has been estimated that the venous origin impacts 5075% of chronic leg ulcers, and this percentage heavily increases if foot ulcers are excluded. These numbers are strictly linked to the fact that signs of CVD could be observed in at least 25% of the population, thus increasing the probability to diagnose CVD /CVI also in patients affected by other forms of ulcer .
Besides the venous origin, other common etiologies are arterial , mixed , neuropathic, diabetic, and pressure ulcers, for which the prevalence reflects overall population aging.
shows the major characteristics of leg ulcer of vascular etiology.
Recommended Reading: Is Ulcerative Colitis A Gastrointestinal Disease
What Can You Do About Vein Disease
At the onset of vein disease, many people seek help from their their primary care doctor. They are often prescribed compression stockings to help alleviate their symptoms.
However, if a person has late stage vein disease, compression stockings may only mask the problem. In fact, we ran a recent survey that indicated that just 9% of people were helped with the use of compression stockings. While 26% of people indicated they received no help at all.
Symptoms Of Venous Leg Ulcer
Symptoms of the early stage of venous leg ulcer are quite different from symptoms of ulcer that has been infected.
Major Symptoms of the early stage of venous leg ulcer include:
- Discoloration around the ulcer site
- Hardened skin around the ulcer site.
- Swollen ankles
Symptoms of the latter stage of venous leg ulcer include:
- Worsening pain on your legs
- Foul and unpleasant smell emitting from the ulcer
- Greenish or unpleasant discharges coming out from the wound.
- You may develop a high fever
Also Check: Ulcerative Colitis Diet During Flare
Skin Grafts And Artificial Skin
Two layers of skin created from animal sources as a skin graft has been found to be useful in venous leg ulcers.
Artificial skin, made of collagen and cultured skin cells, is also used to cover venous ulcers and excrete growth factors to help them heal. A systematic review found that bilayer artificial skin with compression bandaging is useful in the healing of venous ulcers when compared to simple dressings.
Treating Venous Lower Limb Wounds

When treating venous lower limb wounds, it is important to treat the underlying disease, i.e. the chronic venous insufficiency. The aim of the treatment is to improve the impaired return blood flow. The healthcare professional will discuss the treatment options available with the patient. Options may include wound cleansing, wound treatment with wound care dressings, compression therapy with medical compression stockings or adjustable, compression systems, as well as vein operations.
The medi therapy concept for the treatment of venous leg ulcer is based on international guidelines* ** **** as well as medical compression therapy”*. Most importantly, medi products enable patients to participate within their treatment at each phase of their therapy.
Recommended Reading: Arterial Ulcer Vs Venous Ulcer
What Are The Complications Of Untreated Chronic Venous Insufficiency
Several complications may develop should chronic venous disease be left untreated:
- Superficial Venous Thrombophlebitis: When a blood clot forms in a vein that is just under the skin surface.
- Bleeding: This will often be the result of local trauma or injury to the leg
- Lymphedema: The buildup of lymphatic fluid in the tissue beneath the skin.
Signs Of An Infection
A venous leg ulcer can be susceptible to bacterial infection. Symptoms of an infected leg ulcer can include:
- worsening pain
A number of factors can increase your risk of developing a venous leg ulcer, including:
- obesity or being overweight this increases the pressure in the leg veins
- if you have difficulty walking this can weaken the calf muscles, which can affect circulation in the leg veins
- previous deep vein thrombosis blood clots that develop in the leg can damage valves in the veins
- varicose veins swollen and enlarged veins caused by malfunctioning valves
- previous injury to the leg, such as a broken or fractured bone, which may cause DVT or impair walking
- previous surgery to the leg, such as a hip replacement or knee replacement, which can prevent you from moving about
- increasing age people find it harder to move around as they get older, particularly if they suffer from arthritis
You May Like: Signs And Symptoms Of Stomach Ulcers In Adults
Chronic Leg Ulcers: Epidemiology Aetiopathogenesis And Management
Shubhangi Vinayak Agale
1Department of Pathology, Grant Govt Medical College, Byculla, Mumbai 400008, India
Academic Editor:
Abstract
Chronic leg ulcer is defined as a defect in the skin below the level of knee persisting for more than six weeks and shows no tendency to heal after three or more months. Chronic ulceration of the lower legs is a relatively common condition amongst adults, one that causes pain and social distress. The condition affects 1% of the adult population and 3.6% of people older than 65 years. Leg ulcers are debilitating and greatly reduce patients’ quality of life. The common causes are venous disease, arterial disease, and neuropathy. Less common causes are metabolic disorders, hematological disorders, and infective diseases. As many factors lead to chronic lower leg ulceration, an interdisciplinary approach to the systematic assessment of the patient is required, in order to ascertain the pathogenesis, definitive diagnosis, and optimal treatment. A correct diagnosis is essential to avoid inappropriate treatment that may cause deterioration of the wound, delay wound healing, or harm the patient. The researchers are inventing newer modalities of treatments for patients with chronic leg ulceration, so that they can have better quality life and reduction in personal financial burden.
1. Introduction
2. Epidemiology
3. Aetiopathogenesis
| Vascular |
4. Pathogenesis of Chronic Leg Ulcers
4.1. Venous Ulcers
4.2. Arterial Ulcers
4.3. Diabetic Foot Ulcer